Value-based care model shift healthcare reimbursement to tie payment to the efficacy of care and patient outcomes. However, many healthcare organizations need help to make this transition with varying degrees of success. The key to success may lie in the timing, size, and delivery of incentives. Ultimately, these incentives will create a culture of excellence that will drive clinical and operational performance.
Patient Engagement
Patient engagement is a growing healthcare trend that has garnered the attention of many industry professionals. It involves empowering patients to weigh their options and make decisions about their health in conjunction with their physician. This collaborative approach to patient care can lead to improved outcomes and lower costs. While a universal definition for patient engagement does not exist, the concept centers around making patients active participants in their healthcare. This can be achieved in several ways, from promoting a better understanding of disease and treatment to encouraging patients to play an active role in organizational governance and policy-making.
The most common patient engagement strategies include the following:
- Educating and communicating with patients throughout the care process.
- Prioritizing patient feedback.
- Providing relevant education early in the treatment process.
However, implementing these strategies requires actionable data to overcome barriers such as low health literacy and willingness to engage. To help with this, medical software solutions can streamline secure communication between patients and physicians and deliver the actionable data organizations need to drive patient engagement.
Shared Savings Models
Unlike the fee-for-service model, value-based care model programs reward providers for saving money or improving the quality of patient outcomes. Those incentives are tied to specific performance metrics and can be delivered through shared savings or gainsharing programs. Providers are more likely to respond to time-limited incentives directly linked to measured outcomes and large enough to be meaningful.
Both shared savings and gainsharing programs have been shown to decrease healthcare spending by lowering utilization through efforts to avoid admissions, reduce readmissions and improve care coordination. However, focusing solely on reducing utilization creates a financial incentive for ACO participants to withhold services or discourage patients from receiving high-cost services, and quality measures do not prevent this.
Despite this, shared savings and gainsharing programs have successfully promoted shifts toward value over volume. To further accelerate the adoption of value-based care, these models should be accompanied by programs focusing on reducing acute costs at the case level. This will require physician groups to adopt a more effective primary care strategy. Those who do can expect to see even greater cost reduction and patient satisfaction gains.
Patient-Centered Care
Value-based care models encourage healthcare professionals to take a more proactive approach to patient health. This includes addressing the social determinants of health (SDOH) and promoting collaboration between patients and clinicians. It also focuses on eliminating the “utilization waste” created by fee-for-service payments that place too much emphasis on how many services are delivered rather than their quality.
A key element of value-based care is patient-centered care, which means you are involved in your healthcare decisions and plans. Your healthcare professional should clearly explain your treatment options and listen to your opinions. It’s important to include your family and friends in this process as they can provide valuable insights. This model also acknowledges that patients’ cultures, beliefs, and values may influence their healthcare decisions. For example, respecting a patient’s religious beliefs regarding death and pregnancy is important. This type of care can help reduce the anxiety often accompanying dealing with a health condition and promote better outcomes.
Accountable Care Organizations (ACOs)
ACOs are networks of healthcare providers who share financial and medical responsibility for a group of patients. They can coordinate care across the continuum to reduce duplication and prevent waste, including unnecessary or redundant tests and procedures. Physicians in an ACO are incentivized to deliver coordinated care and improve patient outcomes through incentive payments and financial risk arrangements. In these arrangements, ACOs earn shared savings payments if they can achieve cost savings over a performance period compared to the financial benchmark set by payers. However, many smaller healthcare practices may need help to invest in the technology needed to collect and analyze the data required for value-based care. Joining an ACO could provide these physicians with the capital they need to quickly adopt this new way of working, allowing them to deliver better healthcare to their patients.
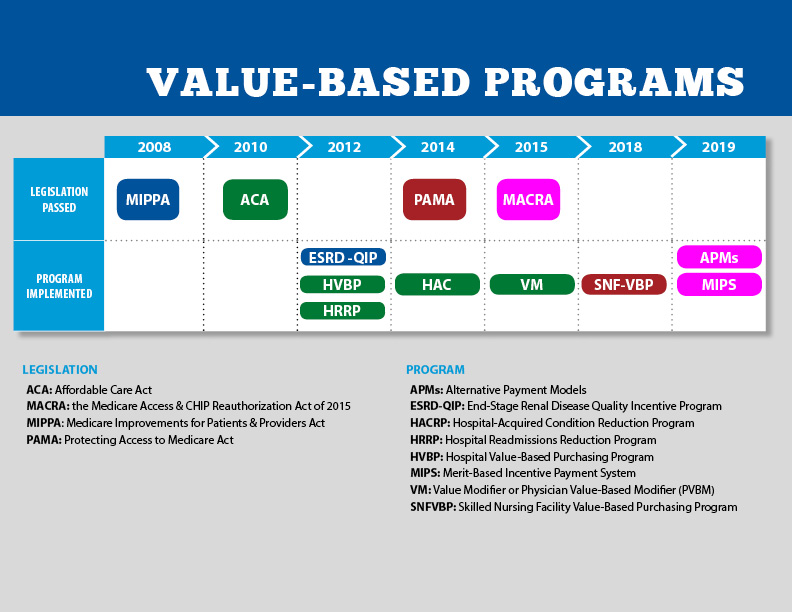
Payment Models
Historically, healthcare providers were reimbursed based on how many services they delivered to patients. This traditional model led to many tests and procedures, often resulting in unnecessary treatments and higher healthcare costs. Value-based care models align reimbursement incentives with the quality of patient outcomes.
The goal is reducing patient harm and improving population health through innovative payment and care delivery models. These programs shift focus from volume to measurable outcomes, allowing healthcare leaders to increase efficiency and drive cost savings. Many value-based care models, such as the Medicare ACO model and the bundled payments in the MSSP program, provide financial incentives for providers if they meet certain performance goals related to improving quality and cost measures. These goals include safety, patient focus and equitability, timeliness, effectiveness and efficiency, and affordability.